Recently, many new data have emerged that testify to the potential of modern therapeutic strategies in the treatment of depressive disorders due to correction of neurotransmitters (biologically active chemicals) of the brain. In particular, numerous preclinical and clinical studies have shown that disorders of N-methyl-D-aspartate (NMDA) receptors, as well as insufficient activity of gamma-aminobutyric acid (GABA) can be key factors for the pathogenesis of depression. In particular, the excessive activation of NMDA receptors, which is observed with significant stress, causes neurotoxic processes and impaired neuroplasticity, then GABA regulates inhibitory mechanisms of mood and emotions. Therefore, the modern scientific paradigm is focused on the development of drugs that can simultaneously suppress excitatory processes and activate brake mechanisms in the brain.
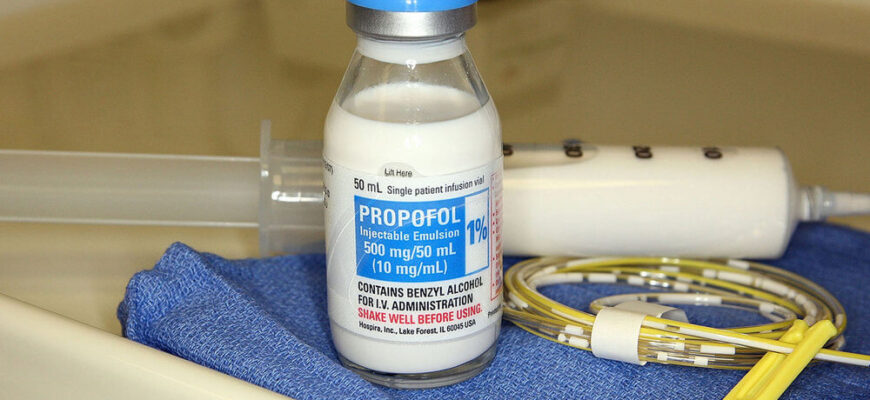
One of the promising tools is propofol - a unique intravenous general anesthetic, which for more than 25 years has been used in clinical practice for procedural sedation and general anesthesia. Propofol acts through several mechanisms: it powerfully potentiates GABA-A receptors, which provides rapid increase in the inhibitory processes in the central nervous system, as well as activates glycine receptors, contributing to synchronization of neural activity. At the same time, the drug suppresses NMDA receptors, which reduces pathological arousal of neurons and can help restore normal neuroplasticity.
Due to its pharmacokinetic features, such as the rapid onset of action and a short erection period, propofol is actively used in outpatient conditions. Its accurate dosage allows you to quickly reach the required level of sedation, and the rapid recovery of consciousness after the procedure provides a high level of safety. The results of numerous clinical studies confirm that the use of propofol has a favorable safety profile, which makes it a valuable tool in clinical practice, even for patients with increased risk of complications.
Depressive people are known to have a significantly reduced brain thickness in the rostral middle frontal gyrus, a paragipcampic gyrus and a posterior belt, and that depressive symptoms are negatively correlated with the area of the island cortex, which plays an important role in the role in physical self -awareness. The last Clinical trials In the US, they indicate the potential for using propofol as an alternative treatment for depressive disorders, especially in cases where traditional methods do not have the desired effect.
The introduction of propofol can provide a rapid improvement in the emotional state of patients, which is likely to be related to the restoration of functional connections in neural networks responsible for mood regulation. It is important that those patients who received high doses of propofol and had the most improvement of symptoms have also had a less decrease in the volume of left hippocampus - a wonderful conclusion that could be associated with the acute anti -inflammatory effect of propofol.
In addition, the study of the use of propofol in PTSD has found that it reduces the long -term disruption of the synaptic plasticity of the hippocampus caused by the PTSD model, and leads to a much faster extinction of traumatic memory, promotes training and recovery after PTSD.
Current studies are focused on optimizing the dosage schemes and the introduction of propofol to maximize its therapeutic efficacy. Integration of this approach into modern clinical practice can open new horizons in the treatment of severe forms of depression and PTSD and promote a significant improvement in the quality of life of patients.
